Our last Breasfeeding 101 post was mainly about demand feeding, which is a very important subject indeed, but one of the first things that must be done when breastfeeding is finding a comfortable position to nurse your baby in. There are four main positions to consider. You may favor one of them over another, or you may choose to use all four, depending on the time of day, or your circumstances. Here are the four main breastfeeding positions:
The Cradle Hold

The cradle hold is one of the most commonly known breastfeeding positions. While using this position you are cradling your baby’s head in the crook of your arm, while holding the baby’s body snugly against yours with that same arm. If you are feeding from the right breast you will cradle your baby’s head in the right arm. The baby’s body is facing you with her chest, stomach and legs resting across or below your opposite breast, either horizontally or at a slight angle. Your forearm and hand are supporting the baby’s spine and bottom.
In breastfeeding all three of my children, I have found this position best used when they are a bit older and have adequate neck and head control. Although the baby’s head is well supported in the crook of the arm, this position does not allow for the mother to have much control of the baby’s head position, which is very important in those first days and weeks of the breastfeeding relationship. Also, if you have had a c-section you may find that this position puts too much strain on your healing abdomen.
When using this position, as with all of the positions, make sure that you are using pillows to prop your arms up if needed. Holding a baby while breastfeeding can cause great strain on the shoulder and neck muscles and pillows will help alleviate some of this strain. If you can, have a stool to rest your feet on as well.
The Crossover Hold

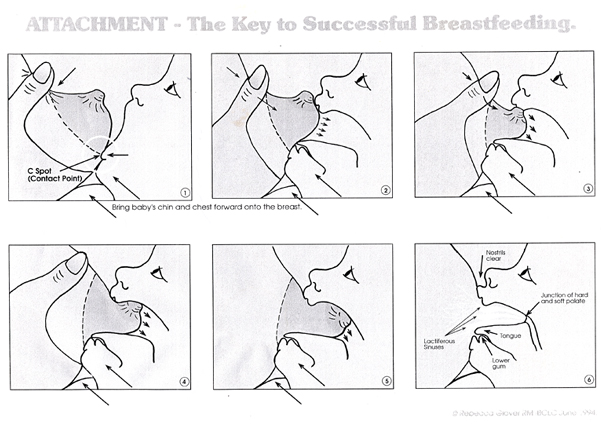
The crossover hold is also called the cross-cradle hold. The crossover hold is a wonderful hold for your first days breastfeeding your newborn, especially if you have a preemie. In this hold, you are cradling your baby to you, but instead of using the crook of your arm to support the baby’s head you are using the opposite hand and arm. The baby is in the same position against your body as it is when using the cradle hold, but if you are feeding from the right side, then the left arm and hand are supporting the baby’s spine, neck, and head. This position is great for newborns and smaller babies because you are able to easily guide the baby’s mouth to the breast (chin first… we’ll discuss this in a future post regarding latching on) and hold it there, as your baby will not have the strength to hold it in position itself.
This is the position that I have always used most frequently with my newborns. It gives me the most control and keeps the baby right where it needs to be to keep a good latch.
The Football Hold
The football hold is also sometimes called the clutch position. In this position you will hold the baby under your arm and to your side, like a football player carries the ball. The baby’s body is held snugly against whichever side you are feeding from, with it’s tummy against your side and its feet behind you, pointing toward your back. Her face will be towards you with her nose lined up with your nipple. It is very helpful to have pillows supporting the baby’s body. A Boppy pillow works great! Just position it around your side instead of your stomach. Support the baby’s neck, shoulders and head with your hand and guide the baby’s mouth to the nipple with your hand, chin first. You may find it helpful to support the breast with your opposite hand.
This position is great for mothers who have had a c-section because there is no pressure on the incision. It’s also a wonderful position for mothers who are tandem nursing twins! If your baby is having trouble latching on this position is very helpful as well.
Reclining Position

The reclining position is a wonderful position for mothers who are recovering from a c-section or for night time feedings. In this position you can cradle the baby’s head with either the top or bottom arm, with his body close and facing you. This position requires pillows to support the mother’s body. Have your partner prop pillows behind you for support, and even place one in between your knees to keep your hips and back in proper alignment. Use a pillow or folded blanket to elevate baby’s head if necessary. You should avoid bending down towards the baby or causing the baby to reach for the nipple.
I found that I used this position more when my baby’s were a bit older, mostly because I am fairly small breasted and so it always seemed difficult for my babies to reach me to nurse when they were very small. However, when they were older this was a great position, especially at night.
I would encourage you to try out all of these positions at some point so that you can decide which works best for you and your baby. Here are some general tips for breastfeeding:
- Alternating breasts that you nurse from first at each feeding helps increase milk production
- It’s a good idea to alternate positions, as each position favors different milk ducts, and using a variety of holds will help reduce the chances of clogged milk ducts
- Create a comfortable space for nursing times. A comfy chair with plenty of pillows at hand, and a distraction-free environment will help you and your baby be able to relax.
- Keep a record of the times that you breastfeed and which side you start on. There are plenty of fun bracelets and even iPhone apps that will help you with this.